More Details
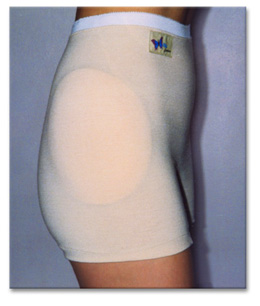
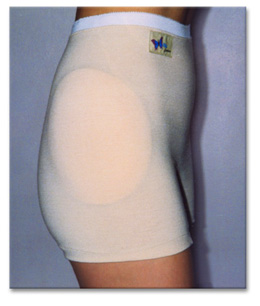
* HipSaver pads are all soft, thin and tapered. The soft padding is encapsulated in an airtight, waterproof pouch. Soft enough to sleep in.
* The viscoelastic foam pads are radio frequency sealed into a high temperature tolerant waterproof pouch.
* When used in a healthcare facility, it is recommended that the hip protector shields are sewn into the underwear to reduce staff effort and time. Sewn in pads can't get lost during laundering or be removed by residents.
* Removable pads are recommended for home use. One pair of pads can be used for several pairs of pants.
* Validated in biomechanical testing and clinical study. Used in more than 5,000 institutions worldwide for over 7 years
Factors To Consider
Hipsaver Program Implementation
* Identify candidates to wear HipSaver hip protector
High risk factors include: Osteoporosis, impairment of gait or balance, orthostatic hypotension, Positive fall history, History of fracture, presence of Neuromuscular disease (Parkinson's, CVA, dementia), generalized weakness, multiple chronic diseases or conditions, medications, dizziness, reduced vision or hearing.
* Assess needs
Determine which HipSaver model is best suited for each person
Considerations: Male / female, toileting ability / degree of continence or incontinence, amount of help needed for dressing, likelihood of backward fall, degree of manual dexterity.
* Determine number of units per person
In a nursing home, the recommended minimum is 4 per resident. Consult with laundry regarding wash cycles. Consider how long it will take for the HipSaver to be returned from the laundry. Residents should wear HipSavers all day, every day and while sleeping. Falls can occur at any time.
* Ensure proper fit and placement of pads
HipSaver hip protectors are designed to position a cushioning pad over the hip bone (trochanter).
* How to determine the location of the hip bone
The hip bone is actually the top of the thigh bone and is shaped similar to a small light bulb. You can feel this bony ball by placing your fingertips on the side of the hip and while raising the knee slightly, noting the movement of the underlying bone. This is not to be confused with the pelvic bone which is higher, more toward the front and does not move when the knee is raised. Fit should be snug to insure proper pad placement.
* Label
Label the HipSaver with the resident's name.
* Educate and encourage compliance
Educate residents and family about serious consequences of hip fracture, note that wearing HipSavers may allow less restraint, more freedom to move about. Demonstrate the softness and comfort of HipSavers. Encourage uninterrupted wear, even while sleeping.
* Ongoing and follow up
Add "HipSaver Wearer" to treatment chart or use the free "HipSaver Wearer" labels available from HipSaver.
* Train clinical staff
Keep records of all falls and any injuries.




 subscribers
subscribers 



